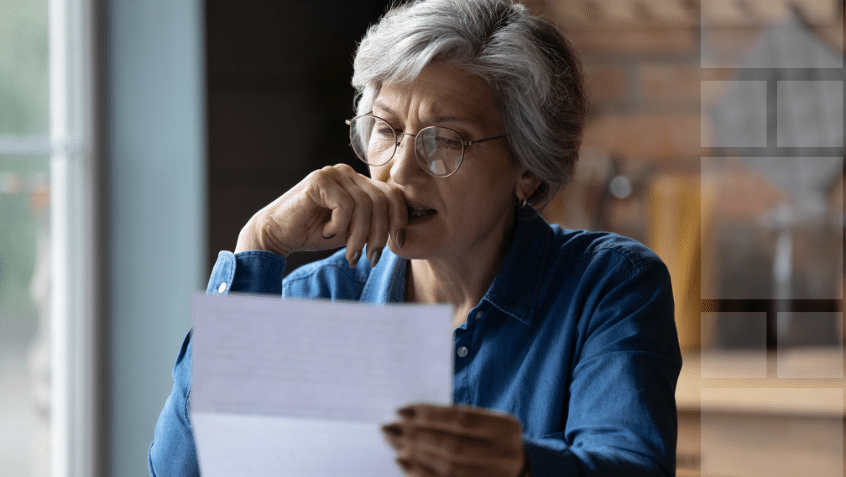
Along with the occasional aches and pains, growing older can bring surprise setbacks and serious diseases. Longtime relationships with doctors people trust often make even bad news more tolerable. Losing that support — especially during a health crisis — can be terrifying. That’s why little-known federal requirements are supposed to protect people with privately run Medicare Advantage coverage when contract disputes lead their health care providers and insurers to part ways.
But government documents obtained by KFF Health News show the agency overseeing Medicare Advantage does little to enforce long-standing rules intended to ensure about 35 million plan members can see doctors in the first place.
In response to a Freedom of Information Act request covering the past decade, the Centers for Medicare & Medicaid Services produced letters it sent to only five insurers from 2016 to 2022 after seven of their plans failed to meet provider network adequacy requirements — lapses that could, in some cases, harm patient care.
Agency officials said some plans lacked enough primary care clinicians, specialists, or hospitals, according to the letters. And they warned that failure to meet the requirements could result in a freeze on marketing and enrollment, fines, or closure of the plan.
CMS declined to detail why it found so few plans with network violations over the 10 years. “The number of identified violations reflects the outcomes of targeted reviews, not a comprehensive audit of all plans in all years,” said Catherine Howden, a CMS spokesperson.
Officials in states with Advantage network violations say CMS didn’t notify them, including directors of the government-funded State Health Insurance Assistance Program, which helps people navigate Medicare.
“It’s hard for me to believe that only seven Medicare Advantage plans violated network rules,” said David Lipschutz, a co-director of the Center for Medicare Advocacy, a nonprofit group. “We often hear from folks — particularly in more rural areas — who have to travel significant distances in order to find contracted providers.”
Medicare Advantage is an increasingly popular alternative to the government-run Medicare program, which covers adults 65 and older and some people with disabilities. Of the 63 million Americans who were eligible to join Advantage plans instead of traditional Medicare, 54% did so for this year. The plans usually offer lower out-of-pocket costs and extra benefits, like coverage for vision, dental, and hearing care, but typically require their members to stick to select networks of doctors, hospitals, and other providers. Last year, the federal government paid Advantage plans an estimated $494 billion to care for patients.
Traditional Medicare, by comparison, has no network and is accepted by nearly all doctors and hospitals in the nation.
Conflicts between Medicare Advantage plans and the doctors, hospitals, and other providers that serve their members are common. Just this year, at least 38 hospital systems serving all or parts of 23 states have cut ties with at least 11 Advantage plans after failing to agree on payment and other issues, according to a review of news releases and press reports. Over the past three years, separations between Advantage plans and health systems have increased 66%, said FTI Consulting, which tracks reports of the disputes.
After March, Medicare Advantage beneficiaries are generally locked into their plans for the year until the annual open enrollment period happening now through Dec. 7, for coverage beginning Jan. 1. But hospitals, doctors, pharmacies, and other health providers can leave plans anytime.
When providers and insurers separate, Advantage members can lose access to longtime doctors or preferred hospitals in the middle of the year. In response, CMS sometimes gives Advantage customers a little-known escape hatch called a “special enrollment period” to change plans or enroll in traditional Medicare midyear.
How CMS decides who gets an SEP is a mystery even to well-versed state insurance regulators and U.S. senators who oversee federal health programs. Oregon Sen. Ron Wyden, the senior Democrat on the Senate Finance Committee, and Sen. Mark Warner (D-Va.) cited previous KFF Health News reporting on Medicare Advantage in an Oct. 30 letter asking CMS Administrator Mehmet Oz for an explanation.
“Despite the serious impacts of SEPs on enrollees and the market, the process of SEP determinations is opaque, leaving enrollees and state regulators in the dark,” they wrote.
“Seniors deserve to know their Medicare plan isn’t going to pull the rug out from under them halfway through the year,” Wyden told KFF Health News.
‘Help Us’
Oz spoke to Medicare Advantage insurers Oct. 15 at a conference organized by the Better Medicare Alliance, a trade group, and encouraged them to help CMS police fraud in the program.
“Be our early-warning system,” he told them. “Tell us about problems you’re witnessing. Help us figure out better ways of addressing it.”
When he finished speaking, he took a seat in the audience next to the president and chief executive of the group, Mary Beth Donahue, and smiled for photos.
In six letters KFF Health News obtained, CMS officials told five insurers that their network adequacy violations could affect Advantage members’ access to care. Five letters listed the number or types of medical specialists or facilities missing from the networks. In three cases, CMS noted that plans could request exceptions to the rules but didn’t. In one letter, CMS requested the plan allow members to receive out-of-network care at no additional cost. Four letters required specific steps to address deficiencies, including submitting evidence that more clinicians were added to networks.
Three letters required a “corrective action plan,” set deadlines for fixing problems, and warned that failure to comply with the rules could result in enrollment and marketing suspensions, fines, or forced plan closure. The other three letters were a “notice of non-compliance,” which urged insurers to comply with legal requirements.
Although CMS regards the letters as the first step in its enforcement process, the agency did not provide information about whether these violations were resolved or if they resulted in penalties.
The Medicare Payment Advisory Commission, a group created by Congress to monitor the program, said in a June 2024 report that “CMS has the authority to impose intermediate sanctions or civil monetary penalties for noncompliance with network adequacy standards, but it has never done so.”
One of the network adequacy violation letters went to Vitality Health Plan of California in November 2020. That came after five hospitals and 13 nursing homes in one county and four hospitals in another all left the insurer’s network, according to the letter from Timothy Roe, then-director of CMS’ Division of Compliance, Surveillance, and Marketing. Two months before sending its letter, CMS granted Vitality plan members a special enrollment period.
Beneficiaries welcomed the opportunity, said Marcelo Espiritu, program manager of the Santa Clara County office of California’s Health Insurance Counseling & Advocacy Program. But Espiritu didn’t know at the time that Vitality’s depleted network violated CMS requirements, which Roe said put “the health of Vitality’s beneficiaries at risk.”
“By not having enough network providers, beneficiaries may not be able to receive necessary services timely, or at all,” Roe wrote.
That’s information patients need to know, Espiritu said.
“People would not be able to receive promised benefits and there would be delays in care and a lot of frustration in trying to find a new plan,” he said. “We would certainly warn people about the plan and remove it from our materials.”
A spokesperson for Commonwealth Care Alliance, which acquired Vitality in 2022, declined to comment on issues that predate the ownership change.
Network Minimums
Federal law requires Medicare Advantage plans to include in their networks a minimum of 29 types of health care providers and 14 kinds of facilities that members can access within certain distances and travel times. The rules, which vary depending on a county’s population and density, also limit how long patients should wait for appointments. The agency checks compliance every three years, or more often if it receives complaints.
Networks can vary widely even within a county because the provider minimums apply to the insurer, not each plan it sells, according to a report from KFF, a health information nonprofit that includes KFF Health News. The company can offer the same network to members of multiple plans in one or more counties or create a separate network for each plan.
In Arizona’s Maricopa County, KFF researchers found, UnitedHealthcare offered 12 plans with 12 different networks in 2022. Depending on the plan, the company’s customers had access to 37% to 61% of the physicians in the area available to traditional Medicare enrollees.
In early 2016, CMS allowed 900 people in an Advantage plan in Illinois run by Harmony, then a WellCare subsidiary, to leave after the Christie Clinic, a large medical practice, left its provider network. The WellCare plan continued to operate without the clinic. But in June 2016, CMS told the plan in one of the letters KFF Health News obtained that losing the Christie Clinic meant the remaining provider network violated federal requirements.
It was “a significant network change with substantial enrollee impact,” the letter said.
Claudia Lennhoff, executive director at Champaign County Health Care Consumers, a government-funded Medicare counseling service that helped the WellCare members, said her group didn’t know about the letter at the time.
“Not disclosing such information is a violation of trust,” Lennhoff said. “It could lead someone to make a decision that will be harmful to them, or that they will deeply regret.”
Centene Corp. bought WellCare in 2020, and representatives for the St. Louis-based company declined to comment on events that occurred before the acquisition.
Two violation letters KFF Health News obtained from CMS went to Provider Partners Health Plan of Ohio in 2019 and 2022. The Ohio Department of Insurance was unaware of the violations, spokesperson Todd Walker said. He said CMS also did not notify the Ohio Senior Health Insurance Information Program, the state’s free counseling service.
Rick Grindrod, CEO and president of Provider Partners Health Plans, which is based in Maryland, said that after CMS reviewed its 2019 network, “we proactively reduced our service area and deferred enrollment in the plan until 2021.”
But Grindrod said the plan enrolled only a small number of members in one county in 2021 and decided to withdraw from the Ohio market entirely at the end of that year.
After Provider Partners withdrew from Ohio, CMS sent it another letter in March 2022 saying its network in 2021 had gaps in four counties for four types of providers and facilities. CMS asked the plan to comply with network rules by adding more providers.
“We believe CMS’ network adequacy standards are generally clear and appropriate for ensuring beneficiary access,” Grindrod said. “While the standards are not difficult to understand, as a provider-sponsored plan with a small footprint, we sometimes face challenges securing contracts with large systems that prioritize larger Medicare Advantage plans.”
In 2021, CMS also sent a violation letter to North Carolina’s Liberty Advantage. CMS didn’t tell the state’s free counseling service, the Seniors’ Health Insurance Information Program, about the letter, said its director, Melinda Munden.
Liberty representatives did not respond to requests for comment.
CMS sent a letter in 2016 to CareSource about network deficiencies in some of its Medicare Advantage plans sold in Kentucky and Indiana. The agency asked the company to fix the problems, including by reimbursing any members billed for services from doctors who were not in the plans’ networks.
“In response to the 2016 violations, we promptly implemented a Corrective Action Plan, which included a thorough review of our provider network to ensure adequacy standards were met,” said Vicki McDonald, a CareSource spokesperson. “CMS approved our plan, and no further action was required.”
[email protected],
@susanjaffe