January is when a lot of “set it and forget it” Medicare costs quietly reset, and that can throw off your budget fast. Even if you don’t change plans, your premium setup can shift because of national rate updates, income-based surcharges, or how your plan bills you. The smartest approach is to treat early 2026 like a quick financial tune-up, not a surprise you deal with at the pharmacy counter. Medicare premium changes are easier to manage when you know which ones are automatic and which ones depend on the choices you made during enrollment. Here are six premium shifts worth checking now so you’re not scrambling later.
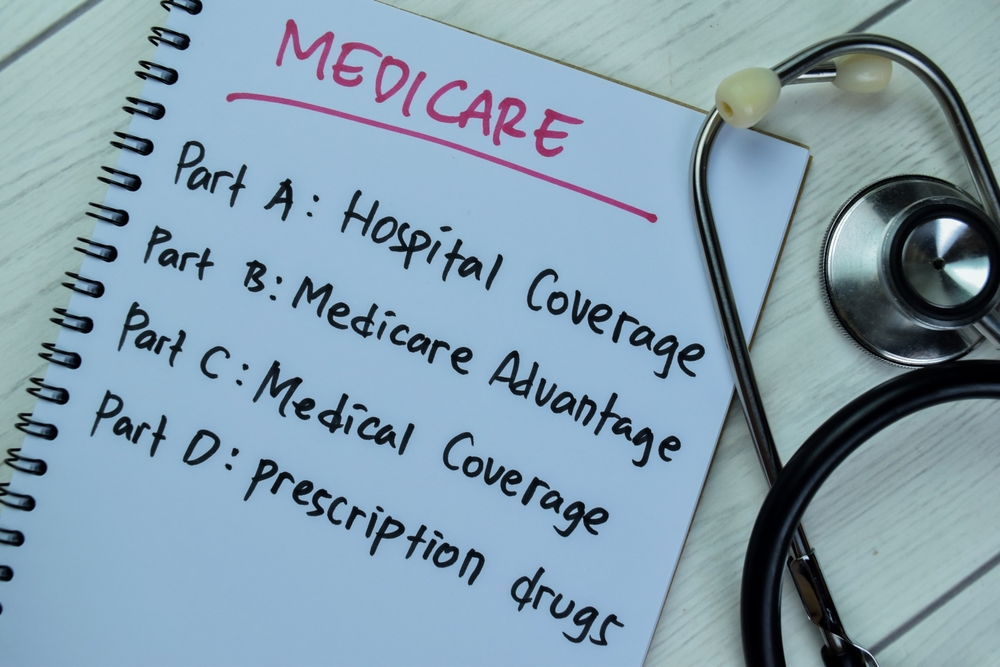
1. Medicare Premium Changes Start With Part B’s Standard Rate
The standard Medicare Part B premium for 2026 is $202.90 per month, up from $185.00 in 2025. If your Part B premium is deducted from Social Security, the change often shows up immediately in your first January deposit. If you’re billed directly, the higher amount can hit as a separate bill, which feels different even when the total cost is the same. Either way, update your monthly budget so the increase doesn’t crowd out groceries or utilities. A quick win is to compare your December and January statements line by line so you can see the real Medicare premium changes.
2. Higher-Income Part B Premiums Can Jump More Than You Expect
Part B premiums aren’t one-size-fits-all, and higher-income beneficiaries can pay a lot more because of IRMAA. For 2026, IRMAA tiers begin when 2024 modified adjusted gross income is above $109,000 (single) or $218,000 (married filing jointly). The CMS table shows total Part B premiums ranging from $202.90 up to $689.90 per month, depending on income tier. If your 2024 income spiked due to a one-time event, don’t assume your 2026 premium will “look normal.” Put a reminder on your calendar to watch for SSA notices so you can verify the tier and catch mistakes early.
3. Part D IRMAA Is an Extra Charge on Top of Your Plan Premium
If you pay Part D IRMAA, you’ll owe that surcharge in addition to your plan’s monthly premium. In 2026, Part D IRMAA amounts range from $14.50 to $91.00 per month, depending on your income tier. The tricky part is that it can be collected differently than your plan premium—CMS notes it may be deducted from Social Security or paid directly to Medicare, depending on your setup. This is why some people think their plan “raised prices,” when the real change is a separate surcharge layer. If you’re near an income threshold, it’s worth rechecking your tax picture so you’re not surprised by the billing method.
4. The Part D “National Base Premium” Changes and Affects Penalties
Even if your plan premium stays steady, the national base amount used in Part D calculations changes for 2026. Medicare lists the national base beneficiary premium as $38.99 in 2026, which is used to estimate the Part D late enrollment penalty. If you’re paying a late enrollment penalty, a higher base can push your total monthly cost up even when no other notable Medicare premium changes apply. This matters most for people who delayed drug coverage without creditable coverage and are now paying the penalty month after month. The practical move is to look at your plan’s premium breakdown and confirm whether a penalty is included. If you spot one, make sure it’s accurate, because a small monthly add-on can become a big annual drain.
5. Part A Premiums Rise for People Who Buy Into Hospital Coverage
Most beneficiaries don’t pay a Part A premium, but if you’re buying into Part A because you have fewer than 40 quarters of covered work, you might see Medicare premium changes. CMS says the reduced Part A premium (for people with at least 30 quarters) will be $311 per month in 2026, and the full Part A premium will be $565 per month. If you’re in this category, that premium is not a small line item—it can rival rent in some areas, so you need it in your budget early. It’s also a good time to confirm whether your quarters record is correct, because errors can be costly. If you recently changed work history, citizenship status, or documentation, verify that SSA has the right information tied to your Medicare eligibility.
6. Medicare Advantage and Part D Plan Premiums Can Change on January 1
If you’re in a Medicare Advantage plan or a standalone Part D plan, your premium is set by the plan—and it can change each year. Medicare notes that Medicare Advantage costs vary by plan and “can change each year,” and your plan’s Annual Notice of Change summarizes what will be effective in January. Medicare also explains that what you pay your plan can only change once a year, on January 1, which is why early January is when the new numbers hit. If you didn’t read your plan notice in the fall, don’t guess—pull it up and confirm your 2026 premium, especially if you use auto-pay. If your premium jumped more than expected, you can still review your options during the Medicare Advantage Open Enrollment Period (Jan 1–Mar 31) if you’re currently in an Advantage plan.
A Simple Early-2026 Premium Checklist That Prevents Budget Shock
Start by confirming whether Part B is deducted from Social Security or billed directly, because that changes how the increase feels in January. Next, check for any IRMAA notices so you can separate income-based surcharges from your base premiums. Then review your plan’s Annual Notice of Change so you know exactly what your Medicare Advantage or Part D premium will be under the new year’s rates. If you pay a Part D late enrollment penalty, confirm whether the updated base premium affects your monthly total. Medicare premium changes are manageable when you treat them like a checklist instead of a surprise.
Which Medicare premium changes worry you most in early 2026—Part B increases, IRMAA surcharges, or plan premium changes you didn’t see coming?
What to Read Next…
5 Medicare Notices That Signal Coverage Reductions Ahead
7 Medicare Appeals That Take Longer to Process in the First Quarter
6 Medicare Advantage Benefits That Shrink After Enrollment Locks
9 Medicare Terms Retirees Misunderstand Every January
6 Medicare Copay Shifts Likely To Hit in Early January